Working on rejected claims is the most important part of revenue cycle management. EZClaim provides multiple tools to help you manage and work on rejected claims.
There are two types of rejected claims:
- Front-end rejections (rejection information found on clearinghouse or payer status reports)
- Clearinghouse rejections due to missing or invalid data.
- Payer rejections due to patient not found or some other issue that caused the claim to be rejected at the 'front door'.
- Payer Rejections (rejection information found on the EOB or 835)
- The claim was processed by the payer but not paid due to reasons provided by reason codes and/or remark codes.
EZClaim effectively manages both types of rejections by offering a comprehensive set of tools that enable the creation of tasks or work lists.
These tools allow for efficient follow-up and ensure proper handling of these claims.
See Online Tutorials for a video on working rejected claims.
To easily navigate this article, use the links provided below. At the end of each section, click "Back to Top" to return to this menu.
Front-end Rejections
One approach to handling clearinghouse rejections would be to print the rejection report, fix the claims, and resubmit them.
Although this method may be effective for a small number of claims, it is not the most efficient system.
EZClaim provides the functionality to process TriZetto CSR (Claim Status Report), ANSI 277, or 277CA reports.
The rejection information is automatically posted to the claim notes, allowing you to easily view a screen of rejected claims. From there, you have the option to promptly fix the claims or create tasks for follow-up at a later time.
Note: The time of the status message is not included in CSR or 277 reports, only the date is provided.
When EZClaim generates claim notes, the time component will be as follows:
Messages with previous dates will be marked as the end of the day at 11:59 PM. Messages with the current date will use the time the message is posted.
This is done to ensure that the messages are properly ordered with other claim activities.
Important: In order to populate the Rejected Claims widget, EZClaim searches for the keyword rejected in the most recent claim note.
Once the biller addresses the rejected claim and updates it, the newer claim note overrides the rejection and removes the claim from the widget.
In some rare instances, the Note Event ID may take precedence over the date/time stamp on a specific claim note.
This might occur when 277CA reports are not opened in sequential order, such as when a more recent report is opened before an older one.
If you are experiencing issues with the Rejected Claims widget not being populated correctly, you can use Find Claim Note and add the Note Event ID column using the Column Chooser.
This will allow you to view the internal number assigned by EZClaim at the time the 277 was processed. The higher the number, the more recent the note.
Additionally, there is a Most Recent Note column available, indicating the most recent note for the entire claim ID in question.
In the example below, for DOS 09/02/2019, two different claims were created, each of which has a unique Claim ID.
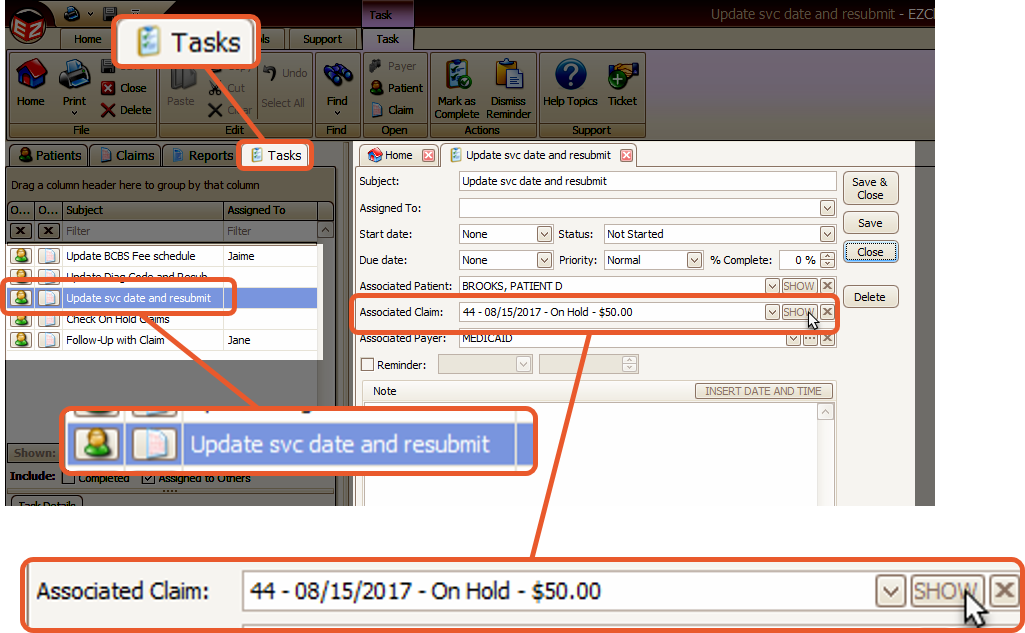
To work your Rejected Claims, we suggested using Tasks. You can find more information about that here.
Claims Not Found
If an attempt is made to read a report that contains claims not found in EZClaim, the following message will appear:
Click Yes to find the missing claims and related information:
Payer Rejections
The workflow for payer rejections (post-adjudicated) differs slightly as the information originates from a separate source.
The following steps will take you through processing an ANSI 835 report and creating tasks for the rejected claims.
See Auto Posting Payments for information on auto-posting payments.
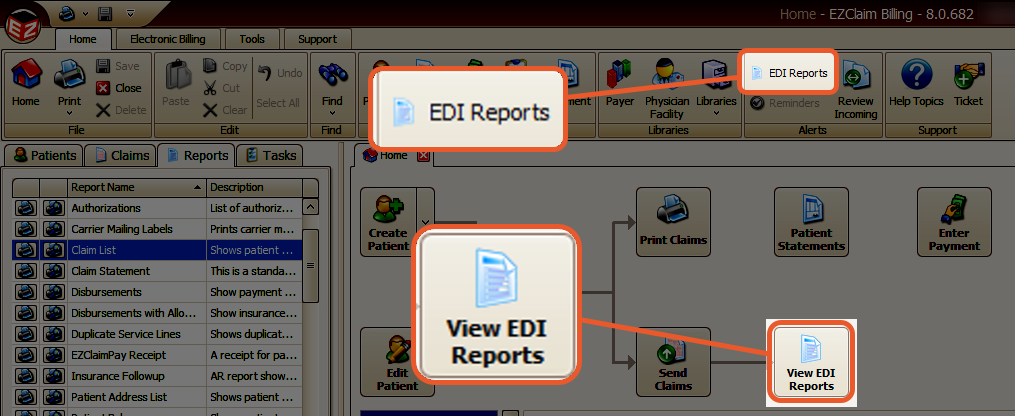
- Click the View EDI Reports button in the Quick Access Menu or the EDI Reports button in the top ribbon bar.
- Download any new EDI reports.
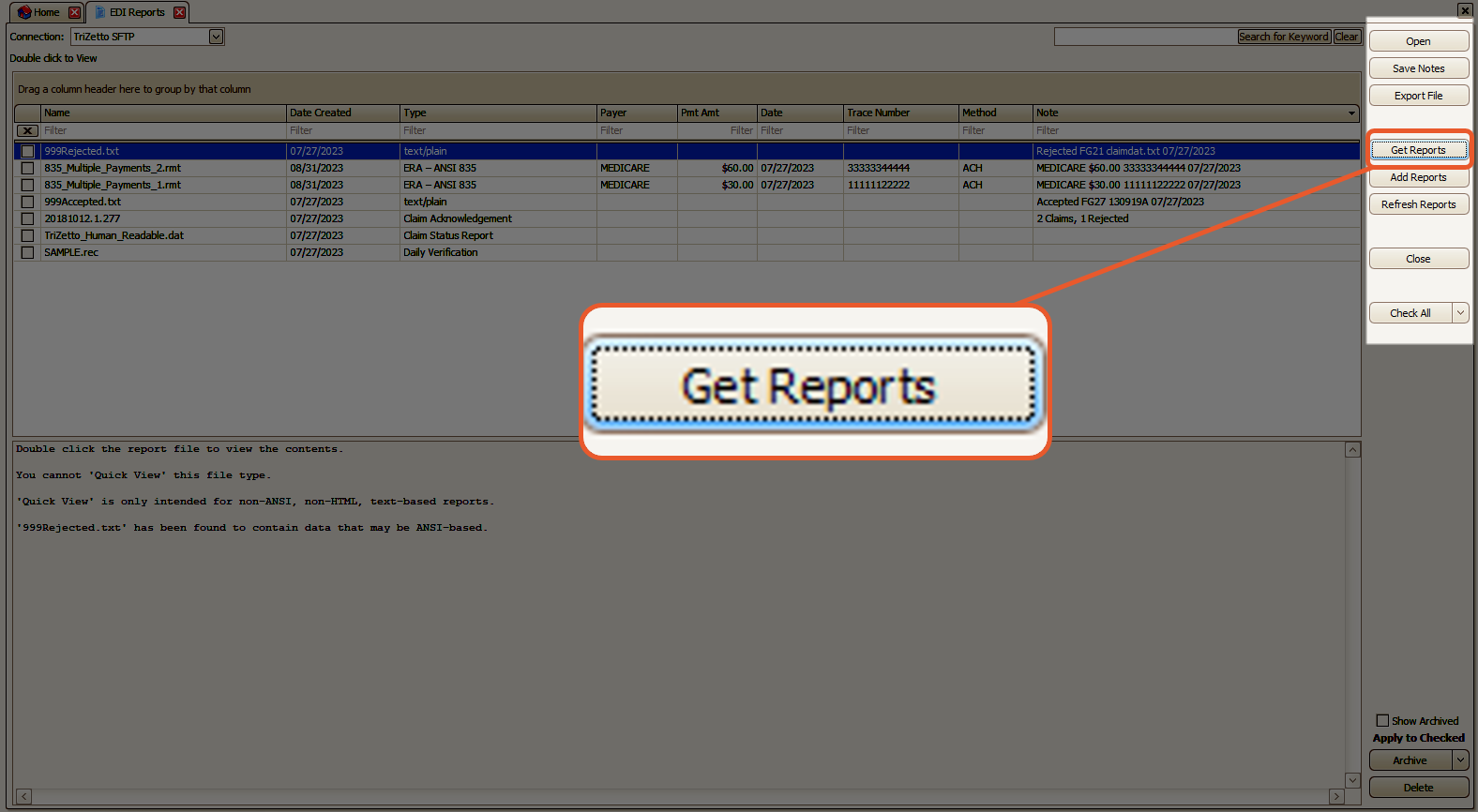
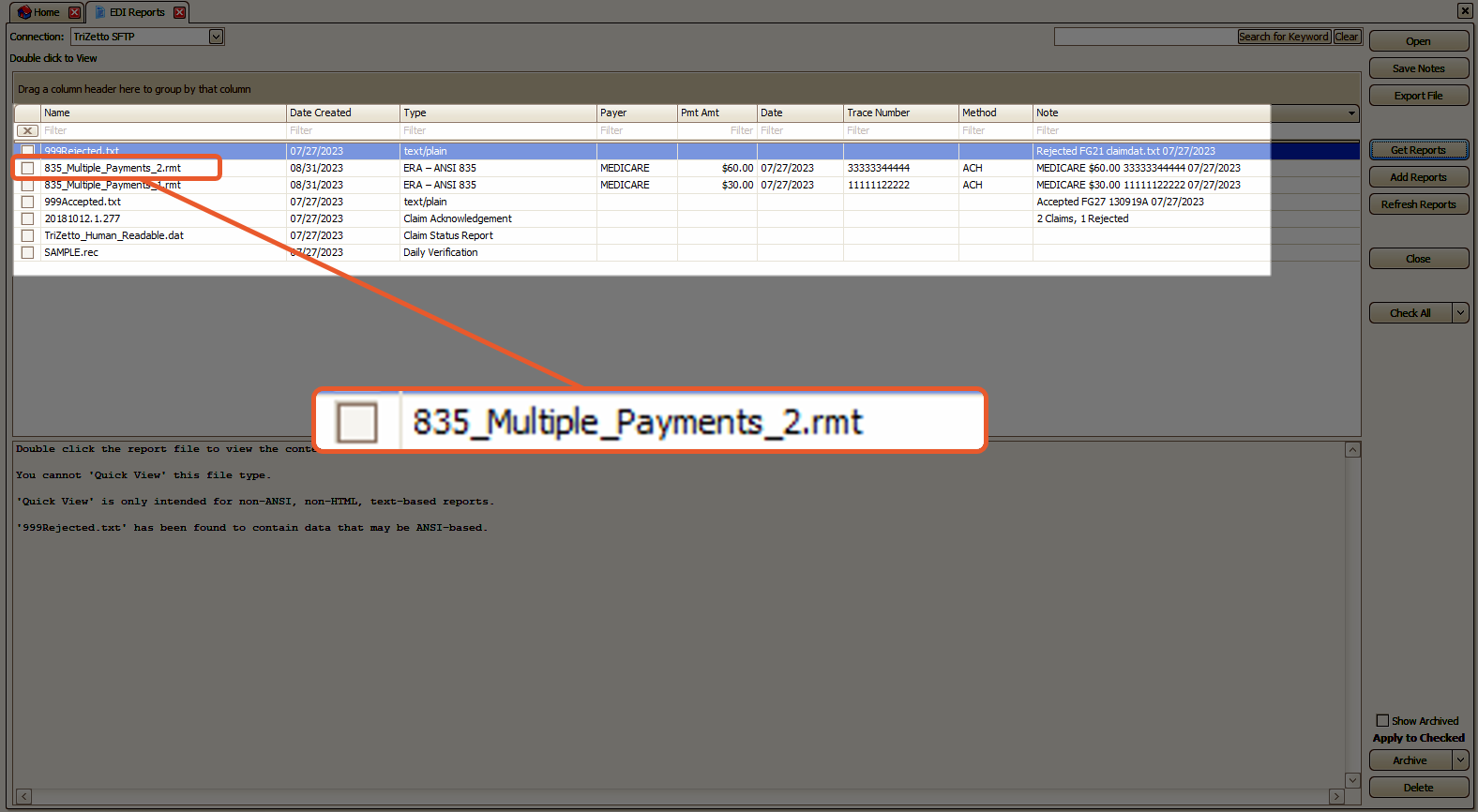
- Double-click the ANSI 835 report
Confirm the selected payer and click OK.
Located at the bottom of the screen, you will find a list of reason codes.
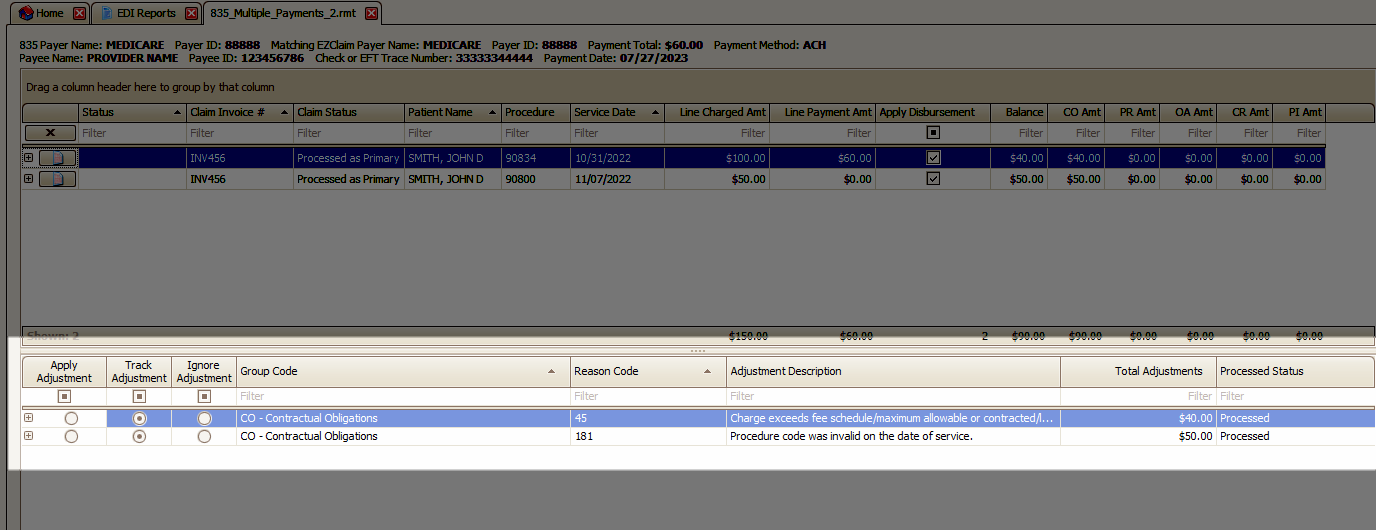
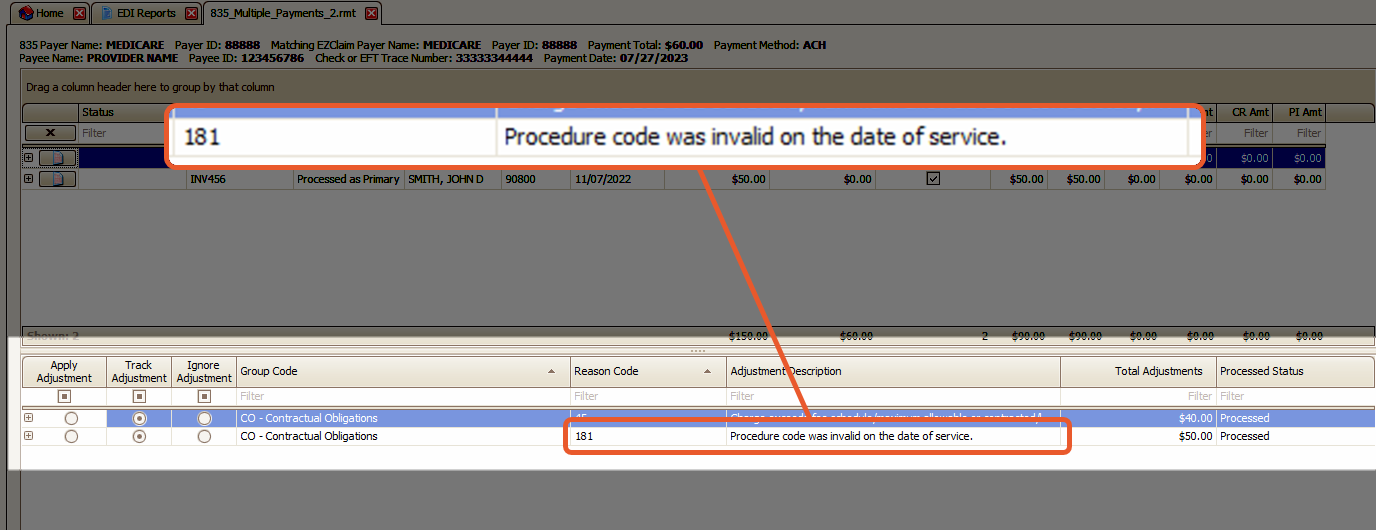
This particular reason code signifies that the claims were rejected due to an invalid procedure code on the date of service. It is necessary to correct and resubmit these claims.
- Right-click the reason code and select Create Tasks Linked to Claims
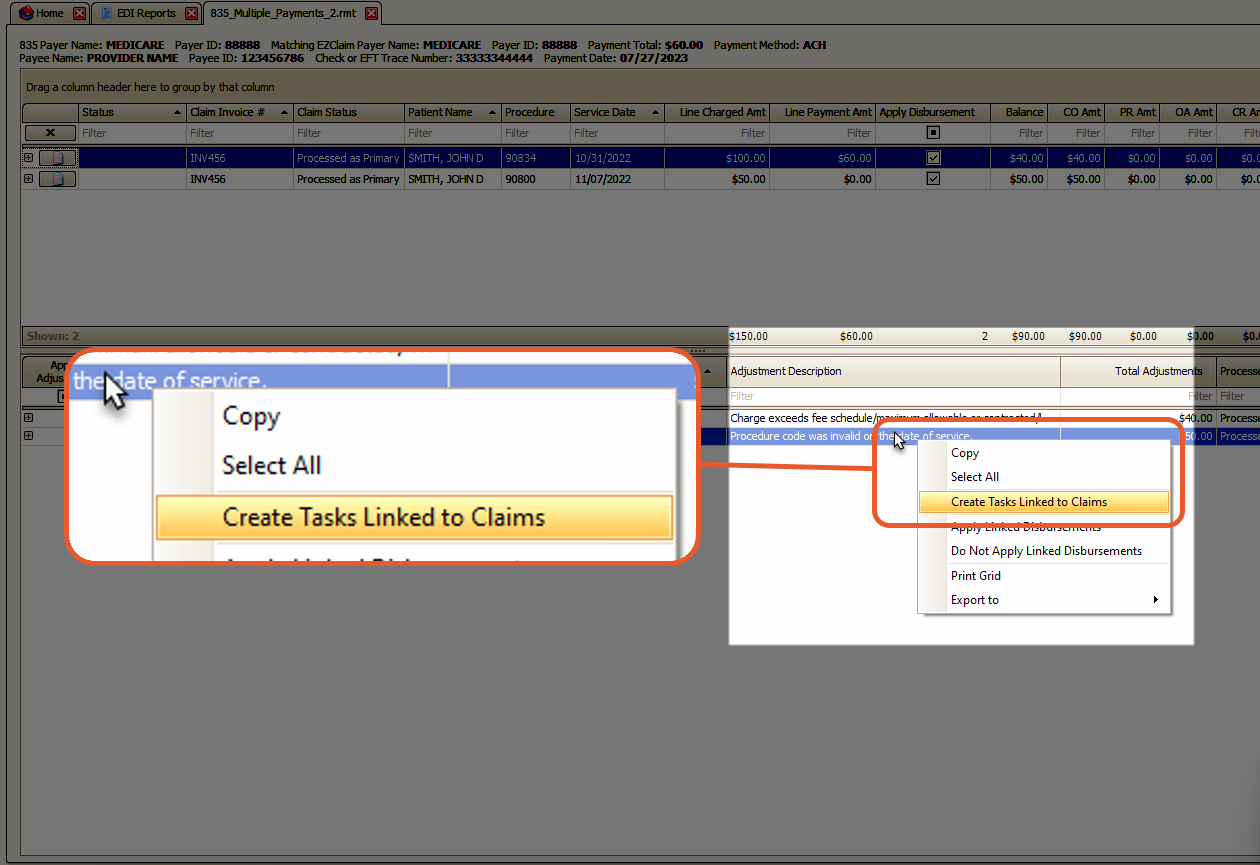
- Fill in the task information and click OK
- Use the Task list to open and work your rejected claims (double-click to open a task. From there you can view the connected claims directly)
Review Resending a Batch of Claims for instructions on resubmitting your claims.