A list of CMS-1500 Boxes and how they interact with EZClaim
To easily navigate this article, use the links provided below. At the end of each section, click "Back to Top" to return to this menu.
CMS-1500 Boxes
Below is the EZClaim logic used for printing data in the following boxes:
- Box 1 - Selected in the Payer Library.

- Box 9a - When printing a Primary claim, this box will be filled with the secondary Group # field. When printing a Secondary (or Tertiary) claim, this box will display both the primary insured’s ID and the primary group number.
- Box 10abc - To populate box 10 fields, enter the information in the fields in the claim grid. Info can also be defaulted in ‘Initial Claim Values’ at the patient level. If added there, remember to update existing claims as needed.
- Two-letter state code is required on all Auto Accident claims.
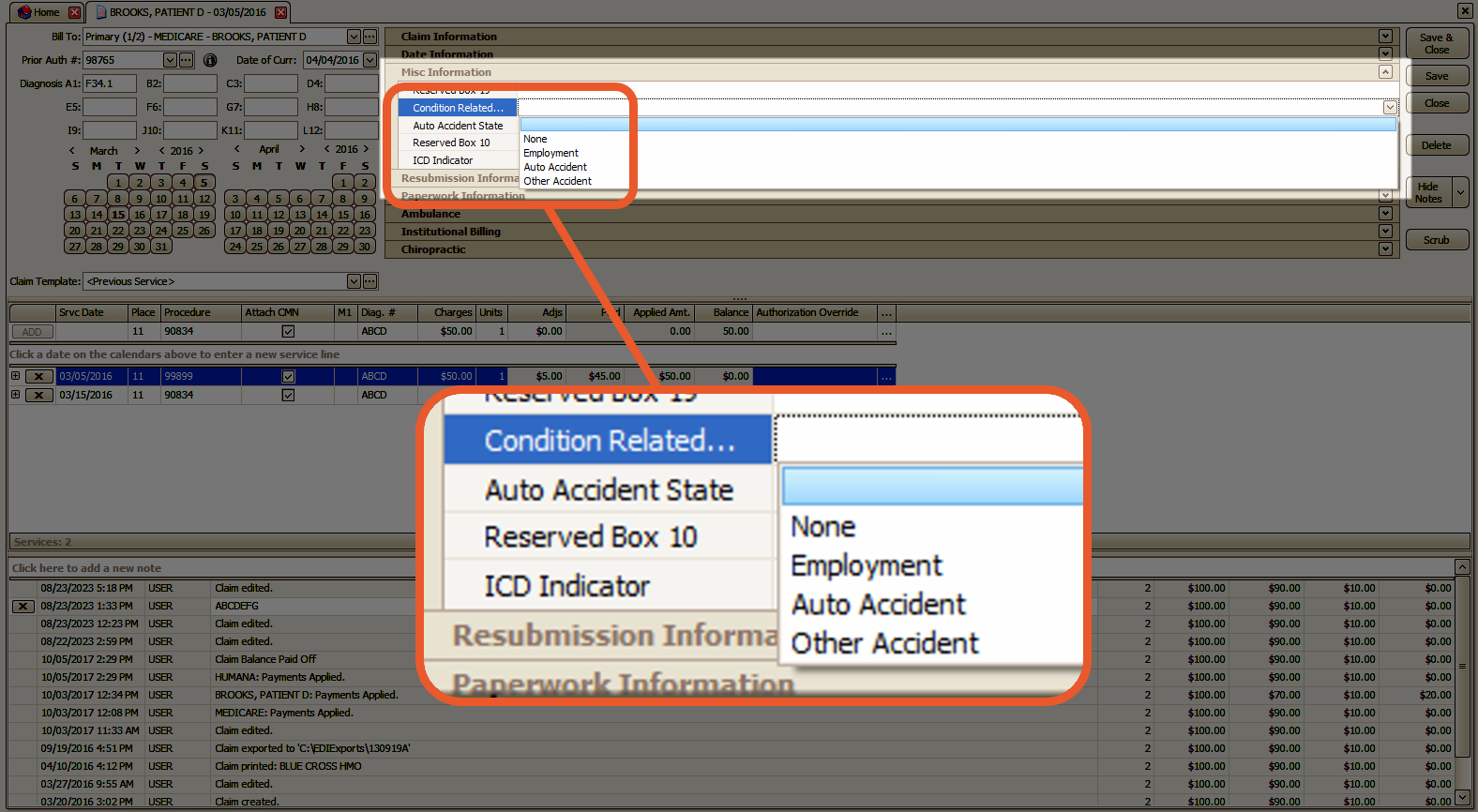
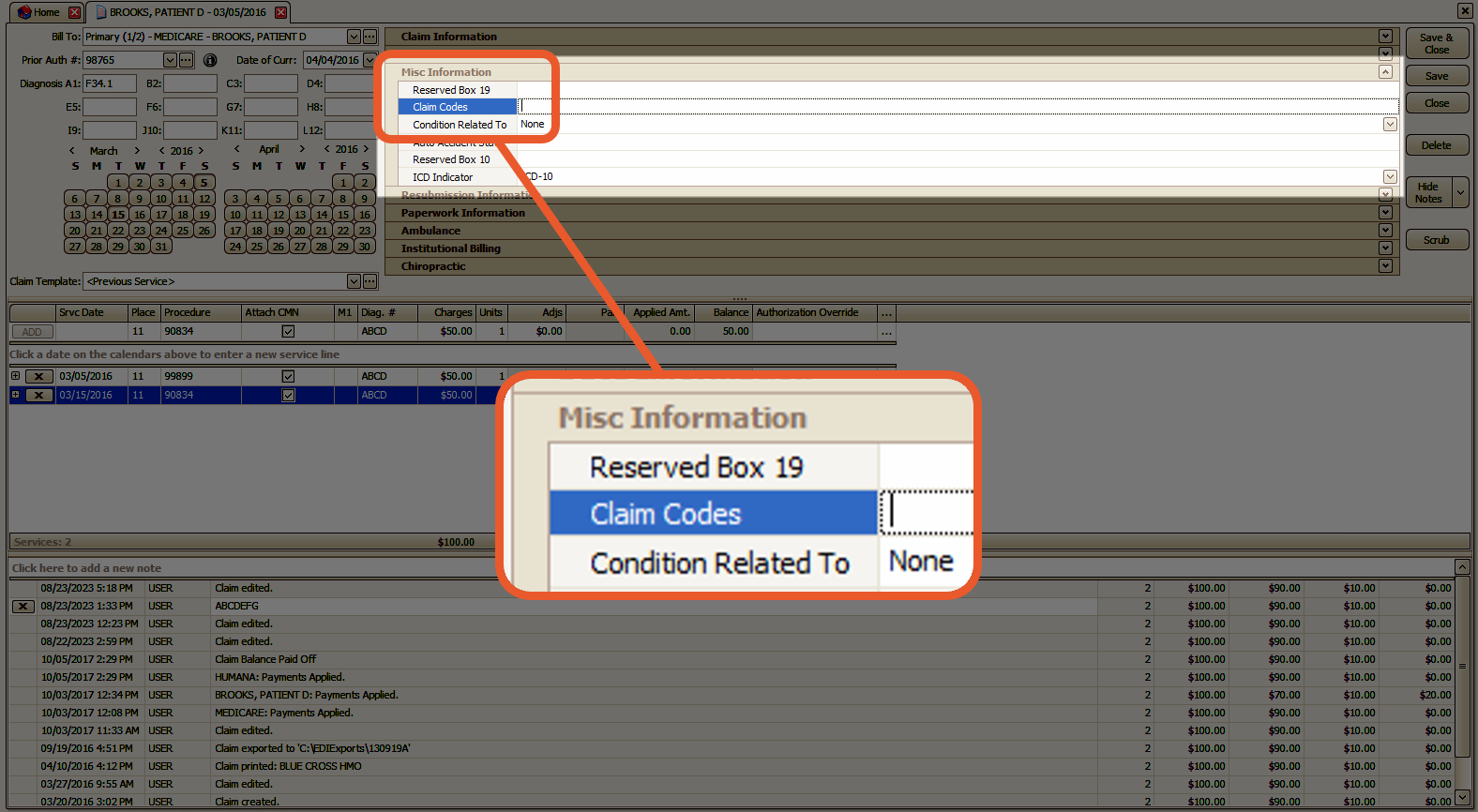
- Box 10d - Claim Codes provide additional information about the patient's condition or the claim itself. It is important to consult the current NUCC guidelines for valid codes and refer to payer guidelines for their specific requirements. This field allows for a maximum of 19 characters.
- Box 11b - This field is used to input the Workers Compensation Claim Number. It may also be referred to as Workman's Compensation, Worker's Compensation, Work Comp, or WC. You can find this field as a custom column on the claim screen's vertical grid. When a WC Claim Number is entered, the qualifier will automatically be set to Y4.
Note: There is no option to change the qualifier
- Box 11d - If the claim has multiple payers attached to it, EZCLaim will automatically select the Yes box. Otherwise, the box will be checked as No.
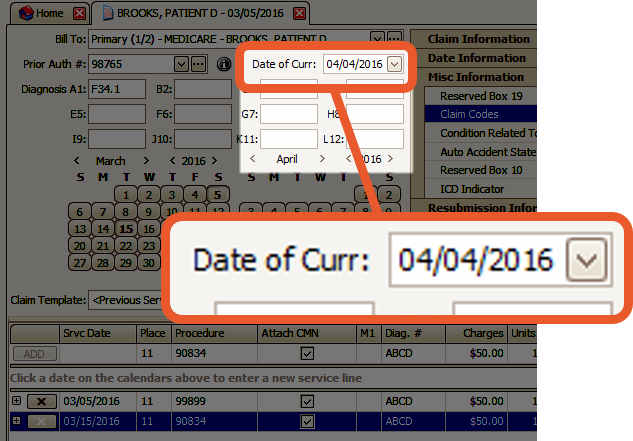
- Box 14 - When filling out the 02-12 version of the 1500 form, you have the option to include different dates in Box 14. The corresponding qualifier will be printed in the QUAL box to the right of the date. EZClaim provides various qualifiers and dates that you can choose from.
If you enter multiple dates, the Date of Current will be given priority.
Note: If the Payer Name field in your Payer Library contains the words MEDICARE, MEDI-CAL, or MEDICAL, the qualifier will not be printed along with the date in Box 14. In such cases, you may need to edit the Payer Name field accordingly.
For example: You can change MEDICARE to NOVITAS or NGS, and MEDI-CAL or MEDICAL can be shortened to MED.
- 431 – Date of Current
- 484 – Last Menstrual Period: This field can be added to the claim grid as needed using the Customize Grid feature.
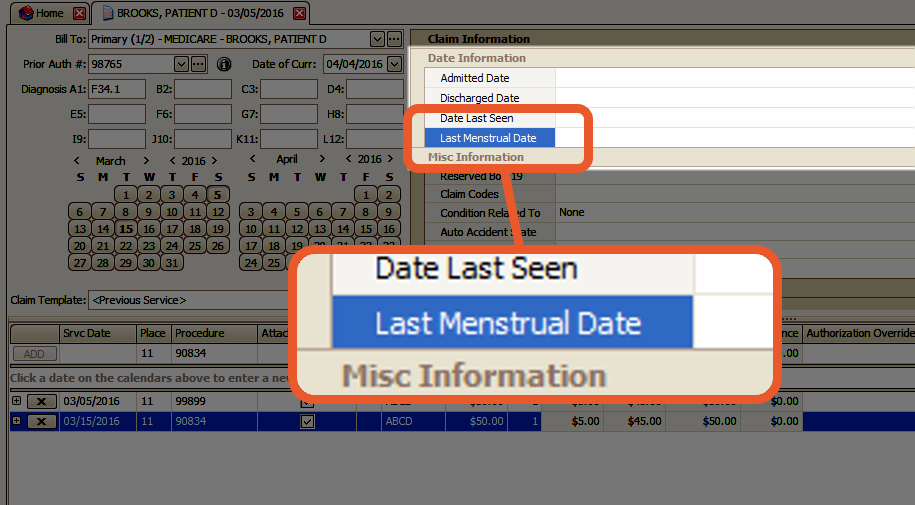
- Box 15 - In the 02-12 version of the 1500 form, you have the flexibility to represent different dates in Box 15. EZClaim provides a range of qualifiers and dates that can be added to the claim grid as required.

Note: Only one date will be printed in box 15
-
- 454 - Initial Treatment Date
- 304 – Date Last Seen
- 453 – Acute Manifestation Date
- 439 – Accident Date
- 455 – Last X-Ray Date
- 090 – Assumed Care Date
- 091 – Relinquished Care Date
Tip: If you do not have the Date Information Category, or date field that you need, right-click and select "Customize Grid". You can find more information on Customizing Vertical Grids here.
- Box 17 - If multiple providers are entered, only the Referring Provider will be printed. In order for the Ordering or Supervising Provider to print in Box 17 on printed claims, the Referring Provider must be removed. EZCLaim automatically generates the following qualifiers, which will be printed in Box 17 and exported in the appropriate loop on ANSI electronic claims.
- DN – Referring
- DK – Ordering
- DQ – Supervising
Tip: To resolve missing qualifiers on printed claims, please check the Payer Library entry for the insurance company in question and ensure that the payer name does not contain Medi-Cal or Medical.
- If necessary, you can abbreviate the name to Med as a viable workaround.
In cases where both Ordering and Supervising Providers are entered, the Ordering Provider will take precedence over the Supervising Provider for printed claim purposes. However, on ANSI claims, both Ordering and Supervising loops will be generated.

- Box 19 - Box 19 is frequently utilized on paper claims to include data that cannot be accommodated on the CMS-1500 claim form. The data entered in this field will be printed on the claim form but will not be exported electronically.
Note: To determine where the payer expects this data, it is recommended to contact them directly. For instance, some payers may expect the data to be included in Loop 2400 NTE*ADD. In such cases, the data should be entered at the service line level in the Service Line Description field.

To add information in Box 19 at the claim-level:
- Use the Customize Grid option (right-click > Customize Grid) to add the Reserved Box 19 field.

- Drag and Drop the field to the desired location in the Claim Information Vertical Grid

- Information added to this field will be included in Box 19 on printing claims.
To add information in Box 19 automatically:
If Box 19 for a patient will always include the same information, you can add this information to the Initial Claim Values in the Patient Record.
- Click the Initial Claim Values button

- Click Click here to add a new row area

- The field that you're looking for is called Other: Reserved Box 19
- Enter the Value that you want to appear there
- Hit the Tab key
Save your changes to the patient record.
- Box 22 - For paper claims, you can enter any resubmission code from the drop-down menu based on the requirements of each payer.
Note: Medicare only allows the use of code 1 to indicate an Original claim.
To determine the specific requirements for flagging resubmitted claims, it is recommended to contact Medicare directly.
If you need to indicate a Corrected claim using resubmission code 6, please be aware that this may not be valid for electronic claims according to payer requirements. In such cases, you may need to edit the code to 7 for Replacement or 8 for Void.
Whether submitting paper or electronic claims, it is important to include the Original Ref Number assigned by the payer to the initially submitted claim. This number will automatically populate the field during ERA auto-posting. If you do not have access to this number, you may need to refer to a payer report or contact the payer directly for assistance.
Tip: If necessary, you can add a Box 22 Code Override field to the claim grid using the Column Chooser feature.
- Box 24c - EMG indicator (also called emergency indicator) is a carryover from the older CMS-1500 form and is unlikely to be required on current claims. If needed, however, you can add the EMG field via the service line Column Chooser. Acceptable values are Y or N.
- Box 24d - If the procedure code is the word BLANK, EZClaim will treat it as truly blank and will leave 24d empty.
- Box 26 - The patient account number typically contains the patient account number found on the patient screen. This setting can be changed in the Program Setup > Printing Claims section. See Account Number (Box 26) for more information.
- Box 29 - Box 29 normally shows payments only. If the option Include Adjustments with Payments in Box 29 is checked in the Payer Library, both payments and adjustments will appear in Box 29. Uncheck Include Adjustments with Payments in Box 29 in Payer Library to edit.
Tip: There is also an option on the claim screen Ignore Applied Amount which will cause $0.00 to print in box 29. This is an optional field that can be added to the claim information grid.

- Box 30 - Box 30 is not normally printed per CMS rules. If your payer requires the balance in Box 30, check the Print Box 30 option in the Payer Library.
- Box 31- If the Ignore Rendering Provider option is not selected in the Payer library for the selected Payer on the claim, the name of the Rendering provider displayed on the Claims screen will be printed in Box 31.
-
- If the Signature on File option is checked in the Physician/Facility Library for the claim's Billing Provider, the text SIGNATURE ON FILE will be printed.
Note: The signature on file setting is stored with the billing provider and not the rendering provider because a rendering provider may not be set on the claim.
-
- Bill Date will print when the Print Claim Bill Date is checked on the patient record.

- Box 32- The claim facility will print in Box 32. If the Address Line 2 is populated in the physician library, it will print in Box 32.
- Box 33- The claim billing provider will print in Box 33. If the Address Line 2 is populated in the physician library, it will print in Box 33.
- Box 33b - Box 33b can be sourced from two different locations. Typically, this field contains the Additional ID Number found in the Billing Provider record in the Physician/Facility library.
Tip: Additionally, there is a field available on the claim grid called Box 33b Override which allows the user to manually enter a value into Box 33b
