How to set up EZClaim for Secondary Claims
To set up EZClaim for Secondary Claims, go through each of the following steps.
To easily navigate this article, use the links provided below. At the end of each section, click "Back to Top" to return to this menu.
Patient Information Screen – Step 2
Payer Library – Step 1
Confirm the following:
- Both the Primary and Secondary Payers have the correct Payer ID numbers
- If the Secondary Payer is Medicare, double-check that the Medicare Secondary Insurance Type Code is selected

Patient Information Screen – Step 2
Confirm the following:
- Secondary Insureds Name, DOB, and Gender are entered
- Secondary and Primary Insurance with Payer ID and Claim Filling Indicator is selected
- Secondary Insureds ID# is entered in the Insureds ID field
- If Medicare or Medicaid claims, the Group field must be blank
- For Medicare Secondary, the Plan or Program Name must be blank
- Secondary subscriber Relationship Code is selected
- SSN and Patient Member ID number must be blank See Other Patient Information
Claim Screen – Step 3
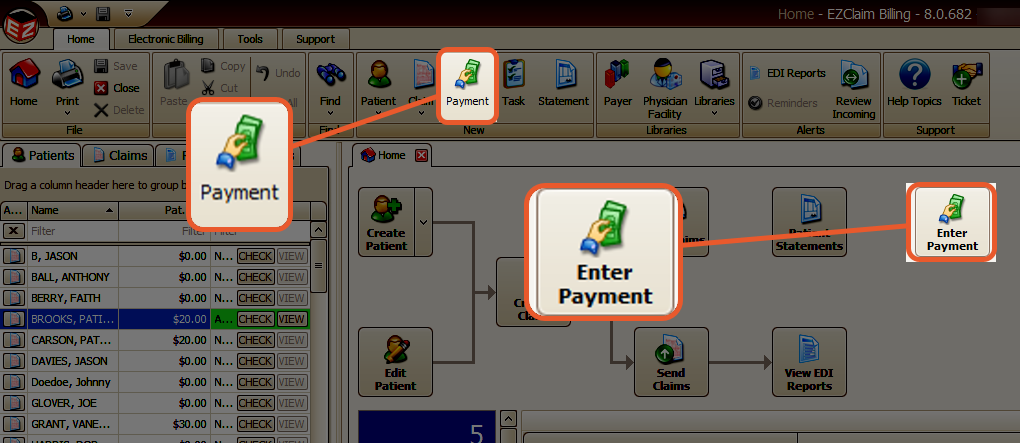
If your payments were not automatically recorded using the Auto-Posting feature, you will need to manually enter payment information from your Primary Explanation of Benefits (EOB). To do this, navigate to the Home → Enter Payment screen.
Confirm the following:
- Payment Entry Screen
- Line Item payments and/or adjustments with a date have been entered on the Payments screen
- Every service line has an Insurance payment entered; even a $0.00 amount must be entered as a payment
- Claim Information Screen
- Bill To has been set to Secondary Insurance
- Ready to Submit is selected under Claim Information: Status

