Not sure what EDI reports are or what to do with them? Read on for the basics of EDI reports and how they can be used in EZClaim Billing.
To easily navigate this article, use the links provided below. At the end of each section, click "Back to Top" to return to this menu.
Overview of the EDI Reports Window
General Information
EDI Reports are used to transmit patient and claim information electronically, between your billing software, your clearinghouse, and your payer. EDI reports that are sent in ANSI format (the industry standard) can be sent and received in your EZClaim Billing program.
Keep in mind - EZClaim can only process ANSI-formatted files. Some clearinghouses may send a text or human-readable format. If you would like to receive those files in ANSI format, contact your clearinghouse and ask that they update the reports to ANSI formatted reports.
Let's take a look at the most common types of files.
-
- .837 - This file is populated in your billing software and transmits all of your claim and patient information for selected claims. Once you have submitted a file you will want to confirm that the file was successfully received.
- .999 - commonly referred to as a Batch Acknowledgement. This file is created by the clearinghouse or payer and simply confirms that the recipient has either accepted or rejected the .837 file. Consider this the 'delivery receipt'. It does not guarantee payment, it only confirms that the file has been received. Once you have confirmation of the batch receipt, you will want to check the status of individual claims.
- .277 - this is the Claim Status Report, generated by the clearinghouse or payer. This report will provide updates on the claim status as it makes its way to the payer for adjudication. The .277 file may include information from both the clearinghouse and the payer, indicating that the claim has been accepted or that it is being rejected. The file will include details as to who has accepted or rejected the claim as well as the reason for rejections. Claims that are rejected can be corrected and resubmitted.
- .835 - everyone's favorite! The Electronic Remittance Advice (ERA). This file is generated by the payer and is the electronic version of the paper EOB. You will need to enroll for ERAs with your clearinghouse/payers to reap the benefits of auto-posting payments in EZClaim Billing. This report will automatically match up the remittance advice with your claims. If the information received from the payer isn't an exact match, you will be prompted to link the corresponding claim in EZClaim Billing.
EDI reports can seem daunting if you aren't familiar with them. However, the benefits and time saved will make it well worth learning how to use them. After some time, you'll wonder how you ever worked without them!
Overview of EDI Reports Window
The 'EDI Reports' screen is where you can easily view and manage all of your EDI reports. These reports are stored along with your company file, making it convenient to access and organize them.
To access the EDI Reports window, simply click on ‘View EDI Reports’ on the home screen or click the 'EDI Reports' button in the ribbon bar on the 'Electronic Billing' tab.

• Double-click a report in the list to view it
Quick View
If a quick view is available, EZClaim will display it in the lower half of the window.
If the file needs to be processed before viewing, the quick view window will provide instructions to double-click the file and view its contents.
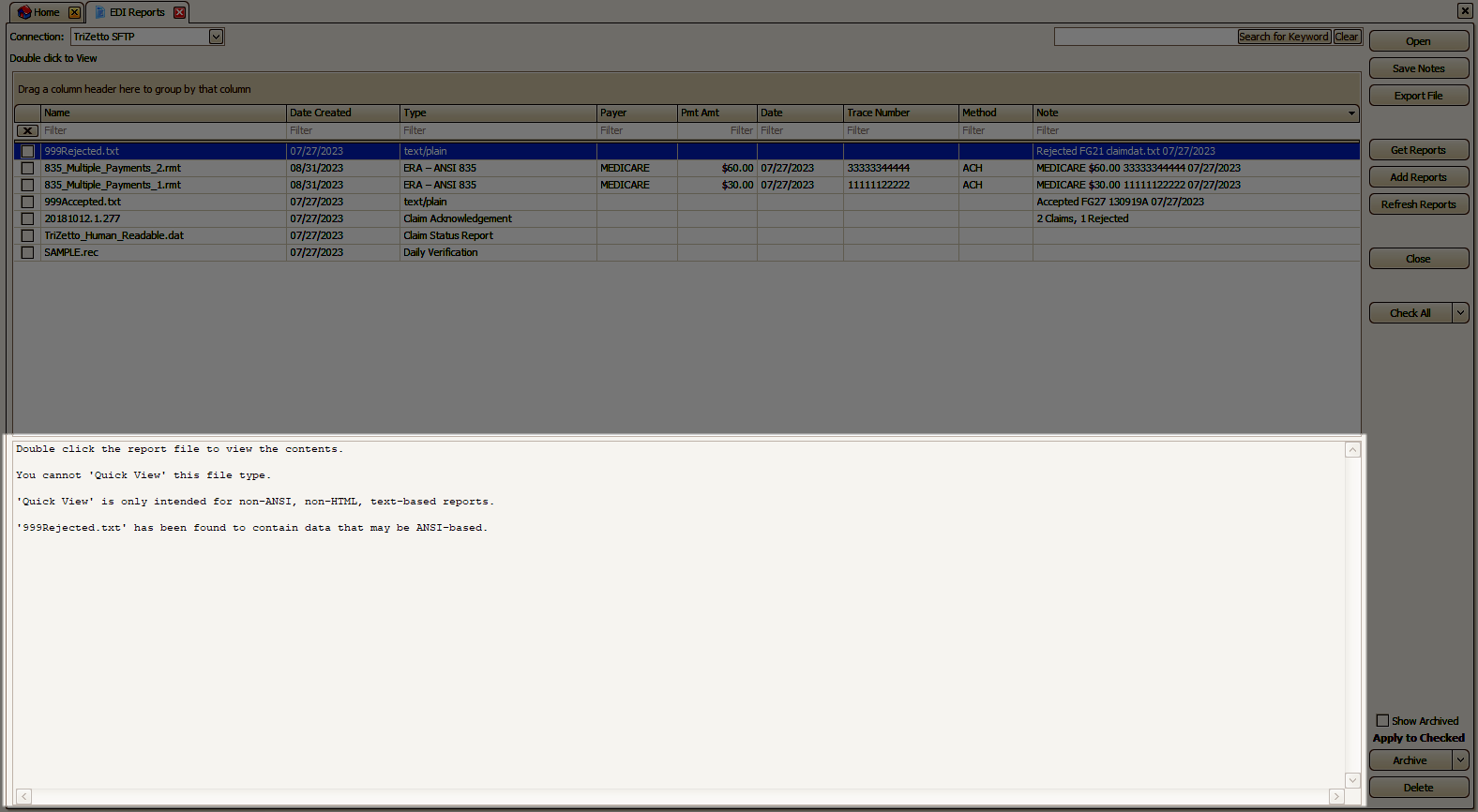
Note: Quick View will only show the first 500KB of data. If the file is too large to preview entirely, you will see the message "[FILE TOO LARGE TO PREVIEW ENTIRELY - DOUBLE CLICK FILE TO ANALYZE]" in the Quick View area.
